Our Surprising Strength: Cancer Research
Andy Tao tempered his expectations when his lab started an experiment to see whether they could identify phosphorylated proteins in blood.
Phosphorylation — the addition of a phosphate group to a protein — is often a precursor to cancer cell formation, but detecting the process would only be half the battle. They needed to correctly identify the phosphorylated proteins in the blood of patients known to have cancer.
“My student, Blair Chen, got the data and immediately came to my office,” Tao says. “She detected over a thousand phosphorylated proteins from 1 milliliter of plasma in a single experiment. She was shocked, and I was totally overwhelmed.”
For years, scientists have searched for biomarkers, measurable substances in the body that correlate with the presence of disease or infection. The promise is the ability to detect cancer, viruses, heart disease and other maladies through a simple blood draw or urine analysis. But success has been elusive.
Tao’s potentially transformative result is one of many success stories in the Department of Biochemistry, which boasts more than half its faculty — 13 of 23 — as members of the Purdue Center for Cancer Research (PCCR). Their work explores many of the complex mechanisms that control cell function and how those can go wrong, with sometimes devastating consequences.
“We have a lot of research going on in cancer,” says Andrew Mesecar, head of the department. “Our degree in biochemistry is broader in scope than many other biochemistry programs at Purdue or elsewhere. Our students come out with a better, in-depth exposure to a wide range of our science.”
As faculty in the College of Agriculture, researchers work with a variety of model organisms — algae, yeast, zebrafish, fruit flies and mice, among others — to understand the basic pathways that lead perfectly normal cells to become cancerous, or cancerous cells that were vulnerable to drug therapies to become hopelessly resistant ones.
“It allows us the opportunity to think more broadly about the basic science of life and all life forms,” Mesecar says. “Here, our scientists are free to explore the commonalities of different organisms. We can identify genes involved in cancer faster in simple systems, identify human gene analogs and apply our understanding to humans quickly.”
the takeaway
- More than half the faculty of the Department of Biochemistry (13 of 23) are members of the Purdue Center for Cancer Research.
- Researchers work with model organisms such as algae, yeast, zebrafish, fruit flies and mice to understand the basic pathways that lead normal cells to become cancerous or cancerous cells to become drug-resistant.
- Several biochemistry faculty members conduct cancer research by studying epigenetic processes, inherited or environmental factors outside of our genetic code that modify how our genes are expressed. This work can help us understand what leads to stable, healthy cells or those that rapidly divide and become cancerous.
- Others examine the enzymes that play a role in cancer, working to inhibit enzymes found at abnormally high levels in cancer, or to help develop drug treatments that bind to enzymes, activating them or shutting them down as desired.
- Professor Andy Tao received Purdue’s 2017 Outstanding Commercialization Award for development of tests that can detect breast cancer in blood and bladder cancer in urine. He is working to develop technology to make the test faster and feasible in standard laboratories.
Shape-shifting RNA
For many years, most scientists have been focused on the role DNA plays in cancer cell formation. But there is growing emphasis on RNA, a chemical messenger that takes instructions from DNA to encode proteins.
The shape of DNA can determine how and when genes are turned on or off in the cell. RNA also changes shape, but since it simply carries DNA’s messages to proteins, few believed RNA’s shape had anything to do with how genes are expressed.
Elizabeth Tran, associate professor of biochemistry, wasn’t convinced. She thought that if RNA could have different shapes and structures, those differences must play a role in the message it delivered to proteins and the resulting gene expression.
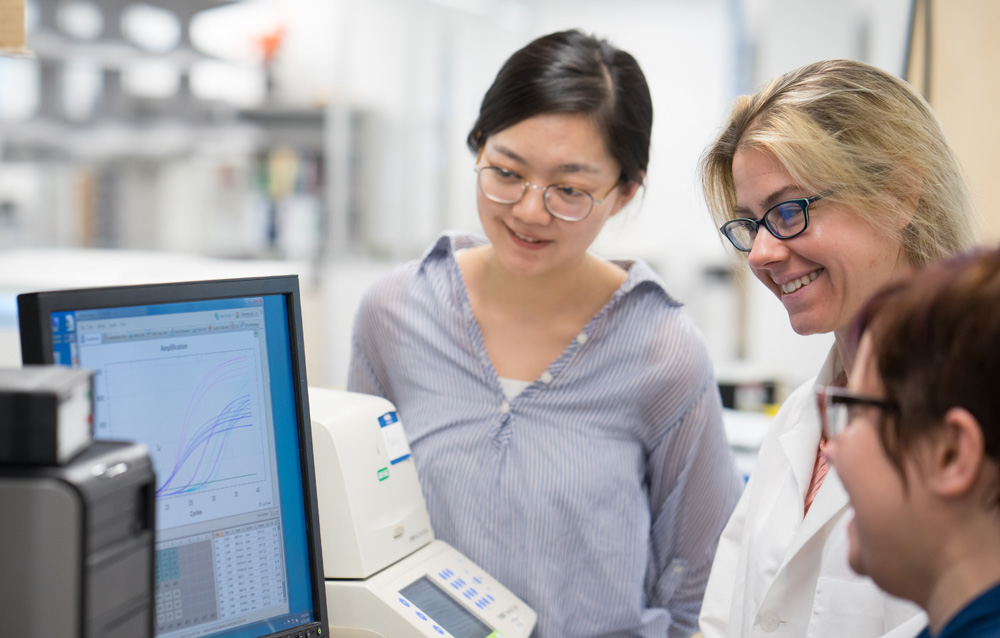
Graduate student Zheng (Cindy) Xing, Associate Professor Beth Tran, and associate researcher Sara Cloutier examine lab results.
Tran decided to examine the role of RNA structure on gene expression by studying a class of enzymes called DEAD-box RNA helicases. These enzymes, found in all life forms from bacteria to humans, bind to and rearrange RNA structures. She used baker’s yeast as a model since it is far simpler than larger organisms and has genes that often correspond to those in humans.
The DEAD-box RNA helicase Tran studied, when present, kick-starts glycolysis, the process by which glucose is broken down and converted to energy.
“Glycolysis is one of the first steps in metabolism that converts glucose to ATP (adenosine triphosphate), giving cells energy. This process also provides carbon building blocks for the cell to allow it to grow and divide,” Tran says.
Unchecked and overactive growth is a clear sign of cancer. And what Tran was seeing in yeast was that a DEAD-box RNA helicase, in rearranging the structure of RNA, was changing the message that encodes proteins needed to break down glucose. Glycolysis and glucose transport into the cell increased, creating the energy needed to induce cancer cell formation.
Having determined what the helicase does in yeast, Tran showed that its function is the same in mammals. Her lab is now looking for novel molecules that can inhibit DEAD-box RNA helicase functions, leading to normal rates of glycolysis. She’s specifically interested in difficult-to-treat cancers such as small-cell lung cancer, which has a five-year survival rate of less than 5 percent, and metastatic prostate cancer.
Professor Xiaoqi Liu studies a form of prostate cancer that's resistant to treatment.
Treating the most intractable cancers
In 1975, a man diagnosed with local or regional prostate cancer, meaning the cancer was in the prostate or had spread to only nearby areas, had a 66 percent chance of living another five years. The odds of beating prostate cancer were far better than the alternative, but the chance of death was still one in three.
Today, cancer treatment progress has pushed the prostate cancer survival rate to 99 percent. Still, that’s not 100 percent, and Xiaoqi Liu, professor of biochemistry, is focused on a group of men with prostate cancer who don’t have great chances.
Fewer than 2 percent of men diagnosed with prostate cancer have contracted a variation of the disease deemed castration-resistant. Many forms of prostate cancer need normal levels of testosterone to grow, but in castration-resistant prostate cancer (CRPC), even when the hormone is reduced to low levels, cells continue to multiply and become drug resistant.
At that point, the only thing doctors can do is buy a little time.
“We have several approaches to try to slow this down, but we don’t have a way to cure it,” Liu says. “Chemotherapy and targeted therapies delay the progression for a while, but only for a year or two at most.”
Liu is focused on an enzyme, polo-like kinase 1 (PLK1), and its role in CRPC and other cancers that are resistant to therapies. PLK1 is known to play a role in cell division and is found at abnormally high levels in human cancers.
His research has found that elevated levels of PLK1 activate androgen receptor, which is a hallmark of CRPC. Inhibiting PLK1 led to a reduction of androgen receptor, and that could be a method for getting these forms of prostate cancer to once again respond to cancer therapies.
“We’ve found PLK1 elevation leads to chemotherapy and drug treatment resistance,” Liu says. “Now, we’re developing PLK1 inhibitors and working with medical school colleagues to start clinical trials to make therapies more effective.”
Leaving the key in the door
Humaira Gowher, assistant professor of biochemistry, is interested in the epigenetic processes — changes outside the genetic code that modify how genes are expressed — that play out as cells differentiate. She wants to understand how enzymes toggle genes off and on, starting cascades that can lead to stable, healthy cells or others that divide out of control and become cancerous.
“Several genes that are expressed in cancer are the same genes usually involved in development during early embryogenesis and the early development of a mammal,” Gowher says. “In cancer, these genes are turned back on. I want to know about the mechanisms that control that process.”
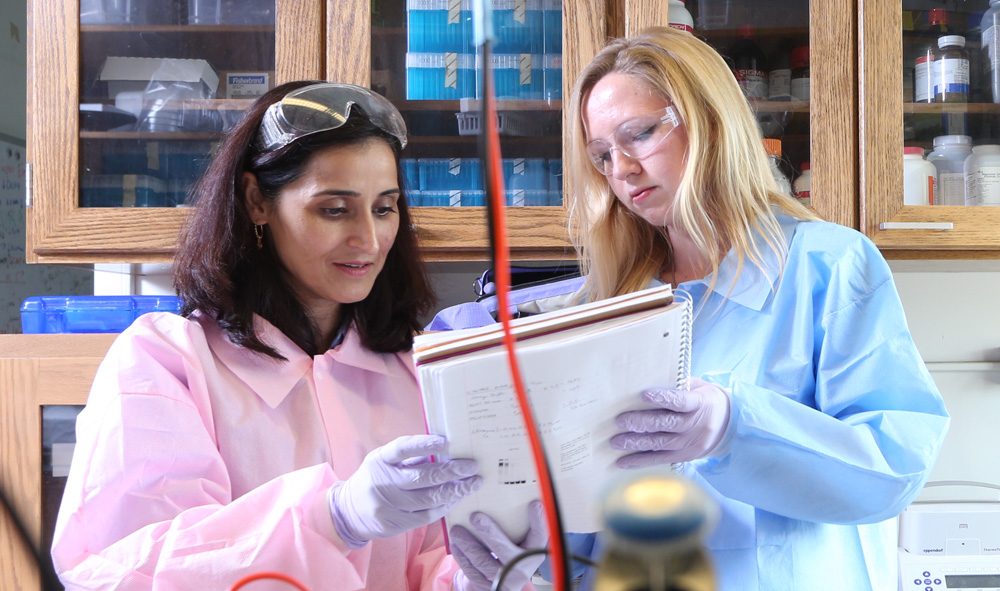
Assistant professor Humaira Gowher reviews the protocol for an experiment with graduate student Allison Norvil.
To understand the research in Gowher’s lab, you have to be familiar with stem cells. They are pluripotent: blank slates that can become any cell type in the human body. They multiply rapidly and are eventually assigned a task, becoming muscle cells, blood cells or some other cell type.
This differentiation occurs as enzymes add and remove methyl groups from DNA and histones — methylation and demethylation — changing the accessibility of the information in genes. This process locks down the cells in a differentiated state and regulates their proliferation. Conversely, loss of the normal enzymatic activity that maintains this stable state can reverse the process and allow those cells to rapidly multiply again, leading to cancer.
Gowher’s work has shown that some cells are ticking time bombs, waiting for the right conditions to turn cancerous because the original cascade of methylation and demethylation hasn’t occurred properly. Instead of completely shutting the genes down, the enzymes only do part of the job, resulting in a gene that’s ready to be activated and primed to transform normal cells into cancerous ones.
It’s like locking the door to the house, but leaving the key in the hole. And it’s a major shift in understanding, because it occurs in a way that hadn’t been seen before: from partial enzyme activity rather than complete loss of enzymatic function.
“It’s not that it’s broken, but it’s only doing half its job,” Gowher says. “It’s leaving it in a state more poised to cause cancer later.”
Gowher will continue to examine molecular mechanisms that cause partial loss of enzymatic activities leading to new or enhanced activity in cancer cells. Her lab has recently received three major grants from the National Institutes of Health, National Science Foundation and American Heart Association to study these mechanisms. Her overarching goal in all of these projects is to understand the role of epigenetic mechanisms, particularly DNA methylation, in development and disease.
Modeling drug discoveries
While leading the Department of Biochemistry, Andrew Mesecar maintains an active research program and serves as deputy director of the Purdue Center for Cancer Research. Since enzymes play such an important role in kick-starting the processes that lead to cancer and other degenerative diseases such as Alzheimer’s, Mesecar studies the 3-D structures of enzymes. This helps reveal how to strengthen the binding of drug molecules to the enzyme, shutting down enzyme activity or ramping it up as needed.
“These enzymes promote the disease process,” Mesecar says. “If we can understand the structures and functions of these enzymes, we can develop therapeutics that can target them and either knock them out or activate them.”
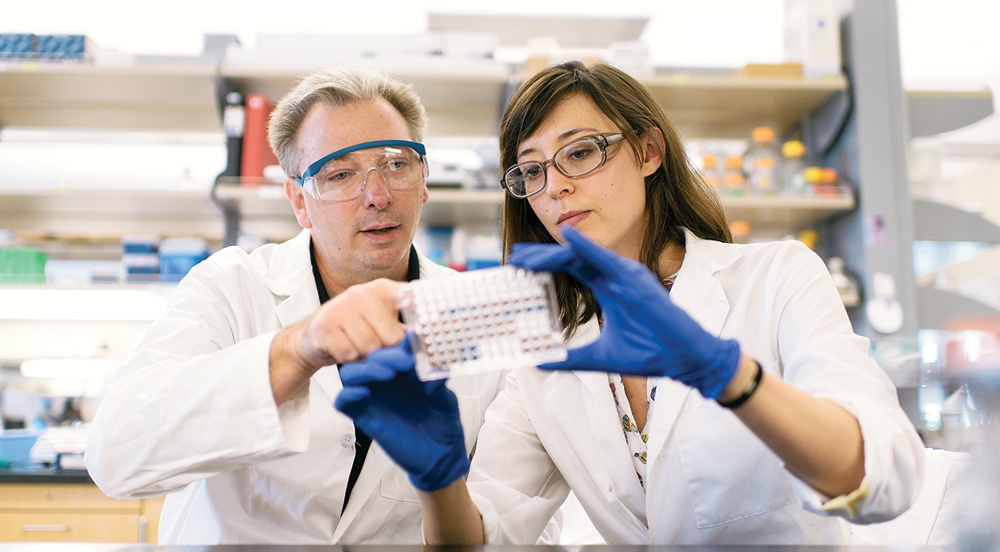
Andy Mesecar, head of the Department of Biochemistry and deputy director of the Purdue Center for Cancer Research, and postdoctoral researcher Renata Everett analyze protein expression levels from cells.
Mesecar is working to develop a small molecule therapy for an enzyme called cholesterol sulfotransferase, which was discovered by Timothy Ratliff , the Robert Wallace Miller Director of the PCCR and distinguished professor of comparative pathobiology, and Graham Cooks, Henry B. Hass Distinguished Professor of Analytical Chemistry. The enzyme promotes proliferation of prostate cancer cells in castration-resistant prostate cancer.
Mesecar developed a novel biochemical assay that allows him to test the enzyme’s activity. From there, his lab tested more than 20,000 small molecules using robots to discover those with potential to disrupt the cholesterol sulfotransferase enzyme.
From those initial tests, a handful might show potential. Using the 3-D models of the enzyme, Mesecar and his colleagues can then synthetically improve the small molecules to make them more effective cancer therapeutics.
“If you know how the molecule interacts with the enzyme, and it isn’t fitting in just right, the 3-D structure allows us to design better compounds to make one work effectively,” Mesecar says. “It allows us to be molecular architects in a way.”
Mesecar is doing similar work with another enzyme, USP7, which is active in multiple myeloma, breast cancer, glioblastoma (a type of brain cancer), and other forms of cancer. He’s in the process of patenting compounds that have shown potential and moving them to animal trials.
Mesecar’s work in drug discovery is at one end of a long cancer research spectrum. Purdue biochemistry faculty touch on points all along the way, from uncovering the complex cellular processes that lead to cancer cell development, to novel methods for detection and therapeutics that promise to give hope to those who once had none.
The quest for easy detection
Doctors can test for a lot of things from a blood draw during an annual physical — diabetes, anemia, and kidney and liver function, along with levels of cholesterol, calcium and other substances. Such testing offers a good look into a person’s health.
One day, cancer might be on that list.
Andy Tao, professor of biochemistry and member of the Purdue University Center for Cancer Research, received Purdue’s 2017 Outstanding Commercialization Award for development of tests that can detect breast cancer in blood and bladder cancer in urine.
Tao and his colleagues identified phosphoproteins in blood plasma that are significantly elevated in cancer patients. These proteins have been phosphorylated, or had a phosphate group added to them, something that often happens during cancer cell formation.
The liver releases phosphatase, which removes the phosphate group from phosphoproteins, making them difficult to find in blood. But Tao used high-speed centrifuges to separate microvesicles and exosomes, which encapsulate and protect the phosphoprotein structure. It’s believed that microvesicles and exosomes, which cells release into the bloodstream, are involved in intracellular communication and metastasis of cancer.
“Our work is the first to demonstrate that many important disease-related molecules can be detected from blood. This can open a new direction for how we achieve early detection of devastating diseases such as cancer,” Tao says. “The technology can also potentially benefit patients who are undergoing treatment by evaluating therapeutic effectiveness of treatment without waiting for long periods of time to monitor whether cancer might come back.”
Tao’s test employed breast cancer cells and bladder cancer cells, but he believes it would transfer well to most types of cancer. His company, Tymora Analytical, is working to develop technology to make the test faster and feasible in standard laboratories.