Mixing fibers for gut health
New Purdue research suggests stronger health benefits for prebiotics with multiple fiber types
Sscientists have long known that fiber feeds beneficial bacteria in the human gut. Now, researches in Purdue University’s College of Agriculture have discovered that combining specific fibers can have a synergistic effect, producing a greater-than-expected number of anti-inflammatory substances. This work has the potential to transform how prebiotics are used to promote health.
Thaisa Cantu-Jungles, a research assistant professor in food science, and Bruce Hamaker, Distinguished Professor of Food Science, recently published their findings in the journal Gut Microbes.
“In the gut, there are so many bacteria related to health,” Cantu-Jungles said. “We selected fibers that promote complementary groups of these beneficial microbes.”
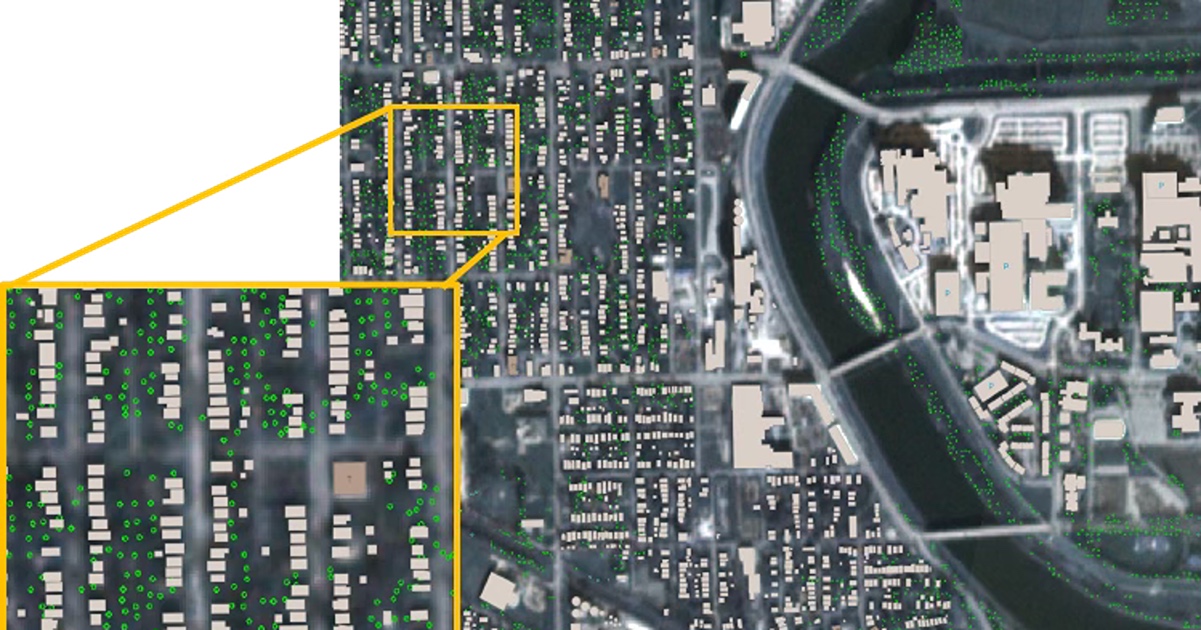
Cantu-Jungles and Hamaker have been working on using fibers to promote specific gut bacteria for years. But they didn’t know how combining fibers would change their efficiency. The 16 fibers they selected for the study were known to promote the growth of bacteria with known health benefits, and to support production of anti-inflammatory short-chain fatty acids. These fibers included pectin, from fruit, and glucomannan, from the root of the konjac plant. The mixture was tested on fecal samples from healthy human adults. The number of beneficial bacteria and metabolites produced was measured and compared to samples using single types of fiber.
“We understood that we can align or match fibers to the requirements that bacteria have for food,” Hamaker said. “But what we found was that when fibers were put together in certain ways, we saw some unexpected things happen.”
These unexpected things can be boiled down to three main findings. First, the fiber mixture generated a higher level of short-chain fatty acids than the sum of the fibers used individually. Second, the mixture produced more beneficial bacteria than expected. And third, the mixture produced a consistent response across individual fecal samples, suggesting it would be effective in individuals with different gut microbiomes.
More beneficial bacteria in the gut can translate into better health.
“About 60% of our immune system is in the gut, and if things go badly out of balance, the gut tends to get inflamed, and the inflammation goes into the bloodstream,” Hamaker said. “Over time, inflammation is related to chronic systemic diseases like diabetes, Alzheimer’s and Parkinson’s.”
Reducing gut inflammation can reduce systemic inflammation and — potentially — prevent or treat disease. Some of Cantu-Jungles and Hamaker’s recent work has shown evidence of these positive benefits. One study showed that a specific fiber mixture can be designed to suppress C. diff, a bacterium that can cause lift-threatening diarrhea. A clinical trial on patients with Parkinson’s disease showed reduced levels of biomarkers for gut and brain inflammation after treatment with a fiber mixture designed for gut-brain axis health. The results were published in the journal Nature Communications. Cantu-Jungles and Hamaker are continuing to conduct research on fiber’s impact on IBS, PTSD and diabetes.
Cantu-Jungles and Hamaker plan to continue experimenting with fiber mixtures to optimize results. Next, they hope to move on to clinical trials with the optimized mixtures. Eventually, they’d like to bring prebiotic supplements to market.
“What we’re looking for in a commercial product would be a prebiotic that acts in a targeted, predictable way, that can make something happen fast,” Hamaker said.
About Purdue University
Purdue University is a public research university leading with excellence at scale. Ranked among top 10 public universities in the United States, Purdue discovers, disseminates and deploys knowledge with a quality and at a scale second to none. More than 107,000 students study at Purdue across multiple campuses, locations and modalities, including more than 58,000 at our main campus in West Lafayette and Indianapolis. Committed to affordability and accessibility, Purdue’s main campus has frozen tuition 14 years in a row. See how Purdue never stops in the persistent pursuit of the next giant leap — including its comprehensive urban expansion, the Mitch Daniels School of Business, Purdue Computes and the One Health initiative — at https://www.purdue.edu/president/strategic-initiatives.
This research is a part of Purdue’s presidential One Health initiative, which involves research at the intersection of human, animal and plant health and well-being.